RABIES
The things you must know
Rabies is an infectious viral disease that is almost always fatal following the onset of clinical symptoms.
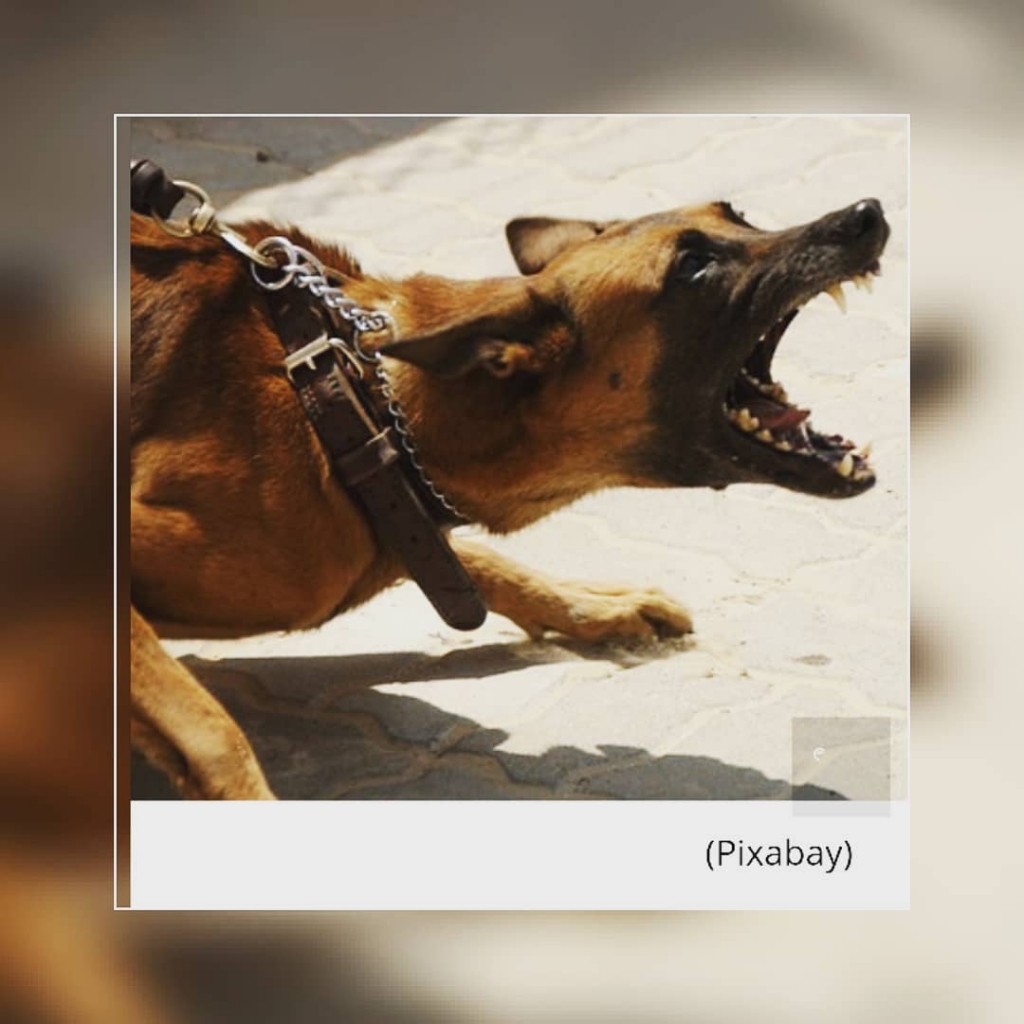
In up to 99% of cases, domestic dogs are responsible for rabies virus transmission to humans.
Yet, rabies can affect both domestic and wild animals such as foxes, bats and raccoons . It is spread to people through bites or scratches, usually via saliva of infected animals.
Rabies is a zoonotic disease. This means that rabies is one of the diseases that animals suffer from and can be transmitted to humans.
Rabies is one of the neglected tropical diseases that predominantly affects poor and vulnerable populations who live in remote rural locations.
Although effective human vaccines and immunoglobulins exist for rabies, they are not readily available or accessible to those in need. Globally, rabies deaths are rarely reported and children between the ages of 5 to 15 years are frequent victims of It.
Every year, more than 15 million people worldwide receive a post-bite vaccination. This is estimated to prevent hundreds of thousands of rabies deaths annually.
Prevention
- Eliminating rabies in dogs
Rabies is a vaccine-preventable disease. Vaccinating dogs is the most cost-effective strategy for preventing rabies in people.
Dog vaccination reduces deaths attributable to rabies and the need for Post Exposure prevention as a part of dog bite patient care.
FarmGrid calls on veterinarians to administer rabies vaccine at a reduced price to enable more people afford to vaccinate their dogs.
- Awareness on rabies and preventing dog bites
Education on dog behaviour and bite prevention for both children and adults is an essential extension of a rabies vaccination programme and can decrease both the incidence of human rabies and the financial burden of treating dog bites.
Increasing awareness of rabies prevention and control in communities should include education and information on responsible pet ownership, how to prevent dog bites, and immediate care measures after a bite.
- Elimination of stray dogs or being careful while getting closer to a stray dog.
Most stray dogs are carriers of this deadly virus. Human beings are therefore advised as a preventive measure, to stay away from stray dogs. Do not approach or talk to them and do not try to scare them. Just avoid them.
- Preventive immunization in people
Human rabies vaccines exist for pre-exposure immunization.
These are recommended for people in certain high-risk occupations such as Veterinarians, laboratory workers handling live rabies and rabies-related (lyssavirus) viruses; and people (such as animal disease control staff and wildlife rangers) whose professional or personal activities might bring them into direct contact with bats, carnivores, or other mammals that may be infected.
Pre-exposure immunization is also recommended for travellers to rabies-affected, remote areas who plan to spend a lot of time outdoors involved in activities such as caving or mountain-climbing.
Symptoms
The incubation period for rabies is typically 2–3 months but may vary from 1 week to 1 year, dependent upon factors such as the location of virus entry and viral load.
Initial symptoms of rabies include a fever with pain and unusual or unexplained tingling, pricking, or burning sensation (paraesthesia) at the wound site.
As the virus spreads to the central nervous system, progressive and fatal inflammation of the brain and spinal cord develops.
Rabies virus is neurotropic, this means that the virus affects the nerves that conduct messages to the brain and spinal cord.
Thus signs typical of CNS (brain) disturbance such as dizziness, hallucinations, muscle spasm or paralysis, mental confusion, seizures, are seen
Diagnosis
Current diagnostic tools are not suitable for detecting rabies infection before the onset of clinical disease, and unless the rabies-specific signs of hydrophobia or aerophobia are present, clinical diagnosis may be difficult. Human rabies can be confirmed intra-vitam and post mortem by various diagnostic techniques that detect whole viruses, viral antigens, or nucleic acids in infected tissues (brain, skin, urine, or saliva).
Transmission
People are usually infected following a deep bite or scratch from an animal with rabies, and transmission to humans by rabid dogs accounts for 99% of cases.
Africa and Asia have the highest rabies burden in humans and account for 95% of rabies deaths, worldwide.
Transmission can also occur when infectious material – usually saliva – comes into direct contact with human mucosa or fresh skin wounds. Human-to-human transmission through bites is theoretically possible but has never been confirmed.
NOTE; Contracting rabies through consumption of raw meat or animal-derived tissue has never been confirmed in humans. But do not attempt to be the first confirmed case.
Post-exposure prophylaxis (PEP)
Post-exposure prophylaxis (PEP) is the immediate treatment of a bite victim after rabies exposure. This prevents virus entry into the central nervous system, which results in imminent death. PEP consists of:
1) Extensive wound washing
This involves first-aid of the wound that includes immediate and thorough flushing and washing of the wound for a minimum of 15 minutes with soap and water, detergent, povidone iodine or other substances that kill the rabies virus.
2) Effective treatment of the exposed patient by trained professionals.
NOTE ; The vaccination status of the suspect animal should not be the deciding factor when considering to initiate treatment. This can be the case if dog vaccination programmes are not being sufficiently regulated or followed out of lack of resources or low priority.

